It is important for
nurses to understand patients' behavior towards health is crucial, comprehend why
patients behave the way they do towards their health becomes pivotal. Enter the
Health Belief Model (HBM), a proven framework that illuminates the complex relation
between beliefs, motivations, and actions when it comes to health.
This article delves into the Health Belief Model (HBM), unveiling its history, its workings, and its significance in promoting patient well-being.
Ticker
6/recent/ticker-posts
Health Belief Model For Nurses and Medical Professionals
POST RN BSN Resources
January 06, 2024
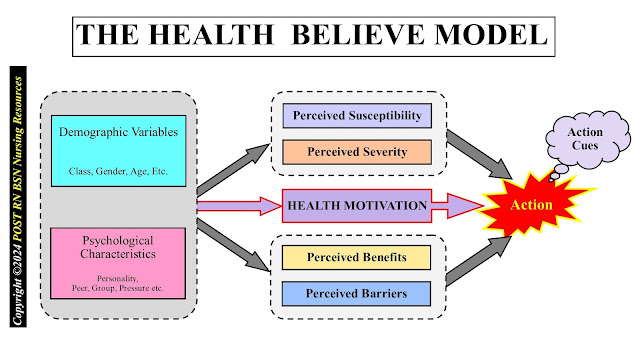
In the 1950s, amidst concerns about low public participation in preventive health programs, this is how Health Belief Model (HBM) developed. Pioneered by Hochbaum, Rosenstock, and Kirscht, it sought to understand the factors influencing why individuals chose specific health behaviors, like vaccinations. Initially focused on understanding vaccination hesitancy, the model's versatility propelled it to encompass diverse health behaviors, offering healthcare professionals a powerful tool for intervention and education.
Imagine the Health Belief Model (HBM) as a mental seesaw. On one side lies the perceived threat of a health condition, its potential severity and personal vulnerability. On the other, rests the perceived benefits of adopting a specific health behavior. Balancing these two sides are two crucial weights: self-efficacy and cues to action.
This two-headed beast comprises perceived susceptibility (the individual's belief in their own likelihood of contracting a disease) and perceived severity (the perceived seriousness of the potential consequences). A smoker who acknowledges the link between smoking and lung cancer but sees themselves as invincible demonstrates a low perceived threat.
Here, individuals weigh the positive outcomes of engaging in a health behavior. A diabetic patient may perceive significant physical improvement and reduced healthcare costs from adhering to a healthy diet, thus enhancing their perceived benefits.
This refers to an individual's confidence in their ability to successfully perform a specific health behavior. A patient apprehensive about using an insulin pump due to perceived complexity will demonstrate low self-efficacy.
These are environmental or interpersonal triggers that prompt individuals to translate their beliefs into action. Reminders from healthcare providers, family support, or public health campaigns can serve as powerful cues to action.
The HBM suggests that an individual's likelihood to engage in a health behavior is a product of these interplaying factors. High perceived threat combined with high perceived benefits and strong self-efficacy, further bolstered by clear cues to action, significantly increase the chances of behavior change.
Armed with the HBM, you can move beyond symptom management and delve into the heart of behavior modification. By assessing a patient's individual perceptions, self-efficacy, and external influences, you can tailor interventions to address specific barriers and motivators.
For instance a cancer patient struggling with chemotherapy adherence. Applying the Health Belief Model (HBM), you can:
Increase perceived severity: Discuss the long-term benefits of treatment, making the positive outcomes tangible.
Highlight perceived benefits: Emphasize the importance of adherence for increased energy levels and improved quality of life.
Build self-efficacy: Offer coping strategies for side effects, provide emotional support, and celebrate small milestones.
Trigger cues to action: Partner with family members to offer reminders, connect the patient with support groups, or explore medication management options.
Through such targeted interventions, you can become a powerful facilitator of behavior change, ultimately leading to improved patient outcomes and well-being.
The Health Belief Model's (HBM) reach extends far beyond individual consultations. Public health campaigns can leverage the model to tailor messaging, focusing on perceived threats and benefits relevant to specific populations. Community initiatives can address self-efficacy concerns by offering accessible health education and skills development programs.
It's important to remember that the HBM is not a static blueprint. Other factors, such as socio-economic status, cultural beliefs, and access to healthcare, can significantly influence health behavior. The model is also evolving, incorporating additional constructs like emotional responses and social stigma to enhance its explanatory power.
The Health Belief Model (HBM) – a valuable tool to unlock the secrets of patients' health choices and ultimately, foster their well-being. By understanding their beliefs, motivations, and capabilities, you can become a skilled navigator of behavior change, guiding patients towards a healthier future.
Post RN BSN Nursing Health Belief Model For Nurses and Medical Professionals | POST RN BSN Nursing Resources
Tags:
Posted by: POST RN BSN Resources
POST RN BSN Resources is a nursing learning blog for RN to BSN, POST RN BSN, Generic BSN and all nursing students and nursing practitioners to have good nursing notes and nursing learning material especially for LUMHS. We are a group of nurses from Karachi. Please contact with your PNC licence no. to join us and encourage the Nursing field for next generation.Followers
About Me

- POST RN BSN Resources
- POST RN BSN Resources is a nursing learning blog for RN to BSN, POST RN BSN, Generic BSN and all nursing students and nursing practitioners to have good nursing notes and nursing learning material especially for LUMHS. We are a group of nurses from Karachi. Please contact with your PNC licence no. to join us and encourage the Nursing field for next generation.
Labels
- Advance Concepts in Nursing – I 4
- BSN 38
- BSN Course 20
- BSN First Semester 17
- BSN Nursing 39
- BSN Nursing ACN – I Course 9
- BSN Nursing Computer Course 1
- BSN Nursing Course Semester 2 2
- BSN Nursing Course Semester 3 2
- BSN Nursing Course Semester 4 3
- BSN Nursing Course Semester I 4
- BSN Nursing English Course 1
- BSN Nursing Microbiology Course 1
- BSN Nursing Physiology Course 1
- BSN Nursing Social Sciences Course 3
- BSN Past Papers 4
- BSN Past Papers Semester 2 1
- BSN Second Semester 2
- Community Health Nursing 7
- Computer in Nursing 1
- Health Assessment 2
- LUMHS ACN – I 4
- LUMHS BSN Course 15
- LUMHS Computer course 1
- LUMHS English course 1
- LUMHS Microbiology course 1
- LUMHS Nursing 29
- LUMHS Post RN BSN Nursing Subjects 1
- LUMHS Professional Development course 1
- LUMHS Social Sciences course 2
- Nurses News 2
- Nursing Assessment 1
- Nursing Career 2
- Nursing Diagnosis 1
- Nursing Process 6
- Nursing notes 6
- PAST PAPERS OF POST RN BSN NURSING 3
- Past Papers 5
- Physiology 1
- Post RN BSN Syllabus 1
- Professional Development 1
- Psychology 1
- RN to BSN 36
- Semester 2 1
- Short Notes 1
- Social Sciences 2
- Sociology and Health 1
NURSING RESOURCES
Popular Posts

Gordon’s 11 Functional Health Pattern
May 09, 2019

BSN Past Papers Semester 1
April 22, 2019

BSN Nursing Past Papers
April 25, 2019

Understanding Health Perception & Helath Management for Nurse
January 24, 2022

BSN Past Papers Nursing Third Semester
April 26, 2019

Past Papers POST RN BSN NURSING Semester 3
April 21, 2019

BSN Past Papers Semester 4
April 24, 2019

LUMHS Post RN BSN Nursing Subjects
April 17, 2019

Post RN BSN Nursing English Course
April 11, 2019

Post RN BSN Nursing ACN – II course
May 05, 2019
Ad Space
Popular Posts

Gordon’s 11 Functional Health Pattern
May 09, 2019

BSN Past Papers Semester 1
April 22, 2019

Understanding Health Perception & Helath Management for Nurse
January 24, 2022
Technology
3/Technology/post-list

POST RN BSN Resources is a nursing learning blog for RN to BSN, POST RN BSN, Generic BSN and all nursing students and nursing practitioners to have good nursing notes and nursing learning material especially for LUMHS. We are a group of nurses from Karachi. Please contact with your PNC licence no. to join us and encourage the Nursing field for next generation
Random Posts
3/random/post-list
 Post RN BSN Nursing
Post RN BSN Nursing
Gordon’s 11 Functional Health Pattern
POST RN BSN Resources
May 09, 2019
Marjorie Gordon was a nursing theorist and professor who proposed a nursing asses…
Recent in Sports
3/Sports/post-list
Recent Posts
recentposts
Popular Posts

Gordon’s 11 Functional Health Pattern
May 09, 2019

Steps to Write the Nursing Diagnosis
May 09, 2019

Celebrations for Pakistani Nurses
May 11, 2019
Contact Form
Search This Blog
Labels
Menu Footer Widget
Copyright ©
POST RN BSN Nursing Resources


5 Comments
When a herpes infection occurs, it typically triggers an outbreak of sores near where the virus entered the body. These sores turn into blisters, which can become painful and itchy before healing. The first herpes outbreak is typically more severe and may be accompanied by body aches, a fever, or swollen and painful lymph nodes. Additional outbreaks typically occur several times a year, though they usually become less frequent over time. I highly recommend Dr. Aboda Nature Treatment Is The Best Way to Treat. Order Via Website https://dr-aboda-solution-home.jimdosite.com/
ReplyDeleteEMAIL drabodasolution@gmail.com
For more info about Dr Aboda you can contact me via: connieluker33@gmail.com
Office , Medical, Educational , Sales Marketing staff
ReplyDeleteI was diagnosed with HSV2 in my eye and mouth, and honestly, I had no idea that it could be transmitted through semen on my face. After enduring two weeks of consistent pain and rashes in my right eye and mouth, I finally decided to get tested and found out I had HSV2. It hit me hard to realize that this had happened to me, especially since I always tried to be careful.
ReplyDeleteTo manage the situation, I started taking lysine and other supplements, avoiding Valtrex because I had heard that stopping it could lead to constant outbreaks. A month later, I added acyclovir eye drops and painkillers, along with various herpes treatments to prevent blindness. For two years, I tried everything to cure myself, but nothing seemed to work.
I started to worry about losing my eyesight and hearing since I learned that herpes could move from the eye to the ears. The thought of losing either was terrifying, especially given my ignorance of the situation, and it began to take a toll on my mental health. To combat this, I pushed myself to attend seminars and anything else that could support my wellbeing.
During that challenging time, I met someone who noticed my sores and recognized them as herpes. She told me that Dr Utu Herbal Cure had worked wonders for her when she faced a similar issue. Intrigued, I reached out to Dr. Utu at drutuherbalcure@gmail.com He reassured me that his treatment would eliminate the herpes from my body. In hopes of improving my mental health, I decided to give it a shot.
Dr. Utu prepared a four week herbal treatment, and to my amazement, it permanently cured me. After undergoing testing again, I was thrilled to find out my results were negative. Now, I'm living free from the fear of losing my eyesight or hearing. I'm no longer fighting depression or anxiety I’ve regained my life thanks to Dr Utu Herbal cure, and I couldn’t be more satisfied 💯
My HSV2 Journey, A Natural Healing Success
ReplyDeleteI was diagnosed with HSV2 14 years ago, and honestly, it was pretty overwhelming at first. I got some info about tablets to help manage the outbreaks, but i was on a mission to find a natural remedy. As someone who loves hitting the gym and navigating the usual life stresses, I was facing outbreaks almost every month that could last for weeks.
I tried just about everything. Tea tree oil? Ouch, that stuff stung like crazy. Lysine? Sometimes it helped, but I had to take over 6000 mg daily, which just left me exhausted. Hot baths didn’t do anything for me either. I noticed that smoking and drinking seemed to trigger outbreaks, so I decided to cut those out since they weren’t doing my health any favors in my mid-30s.
Even regular exercise would lead to more outbreaks, and let’s not even talk about manscaping, definitely a no go. On top of all that, my mood was sinking, and I was feeling pretty down. My sex life was non existent, and I just wanted to feel like myself again. I wasn't a fan of prescription meds, and I was avoiding doctors because, you know, manly reasons. But I finally thought, why not?
After reading some great reviews online about Dr Utu Herbal Cure
, I decided to give it a shot. I reached out through his email at drutuherbalcure@gmail.com and ordered the Herpes Herbal Cleanser. I received the herbal cleanser through DHL and committed to a four week treatment plan.
Fast forward to when I got my blood tested, it came back negative for HSV2! I even went to another hospital for a second test, and once again, NEGATIVE! This was a total game changer for my health, and I can’t believe how quickly 13+ years of depression lifted.
Feeling like myself again has been truly incredible!
Insightful explanation of the Health Belief Model for nurses and medical professionals. St. Mother Teressa School of Nursing, a Good Nursing School in Mirzapur, focuses on teaching such models to help students improve patient education, preventive care, and evidence-based nursing practice. Great and informative content.
ReplyDelete