Nurses spend more time with patients than other health team members, and are crucial care providers of patient focused resources and education. Nurse is the one on which patient depends on, in terms of recovery and guidance. Ironically, professional nurse can provide care in better way by understanding not only the needs but also psychology of patient and their belief of health. Health Belief Model in Nursing Studies gives an opportunity to develop efficient understanding of health belief of a person and why he reacts to prevention and cure of a disease.
The health belief model is a, instrument for nurses, offering outline for helping their patients prevent chronic disease or, improve quality of life during suffering.
Nurses can use this model to explain patients' perceptions of risk and why they behave in a way that is harmful; this enables nurses to apply strategies that empower patients to make healthy lifestyle changes. Patients' perceptions can be affected by age, sex, and personality. patients who are overweight and diabetic or those who have high blood pressure or Cholesterol and eat processed convenience foods high in sodium. Nurses can use the health belief model in any of these conditions.
History and Orientation of Health Belief Model
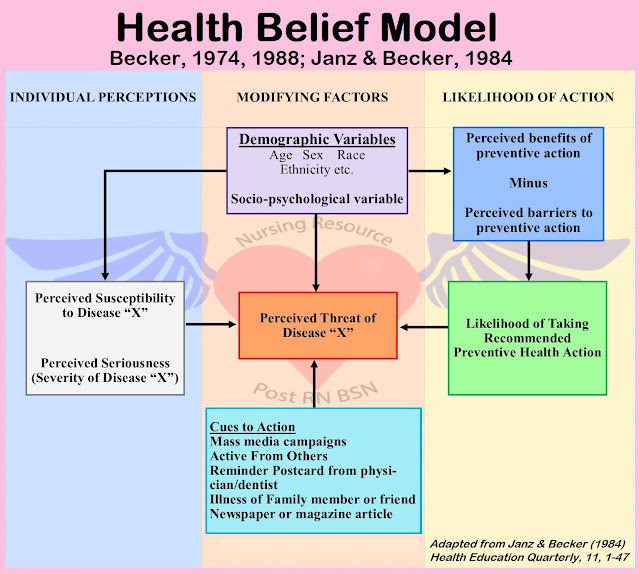
The HBM was first developed in the 1950s by social psychologists Hochbaum, Rosenstock and Kegels working in the U.S. Public Health Services to explain the failure of people participating in programs to prevent and detect disease. Later, the model was extended by others to study people's behavioral responses to health-related conditions.
Actually, the model was developed in response to the failure of a free tuberculosis (TB) health screening program. Since then, the HBM has been adapted to explore a variety of long- and short term health behaviors, including sexual risk behaviors and the transmission of HIV/AIDS.
According to this model, your individual beliefs about health and health conditions play a role in determining your health-related behaviors. Key factors that affect your approach to health include:
- Any hurdles might be standing in a person’s way
- Exposure to information that encourage to take action
- How much of a benefit a person think will get from engaging in healthy behaviors
- How susceptible to illness, a person belief
- What are the consequences will be, of becoming sick in a person’s opinion
- Person’s confidence in ability to succeed
Health experts often look for ways that such health belief models can impact the actions people take, including behaviors that can have an impact on both individual and public health.
Assumptions and Statements
The HBM is based on the understanding that a person will take a health-related action (i.e., use condoms) if that person:
1 - Feels that a negative health condition (i.e., HIV) can be avoided,The HBM was spelled out in terms of four constructs representing the perceived threat and net benefits:
1 - Perceived susceptibility,
2 - Perceived severity,
3 - Perceived benefits, and
4 - Perceived barriers.
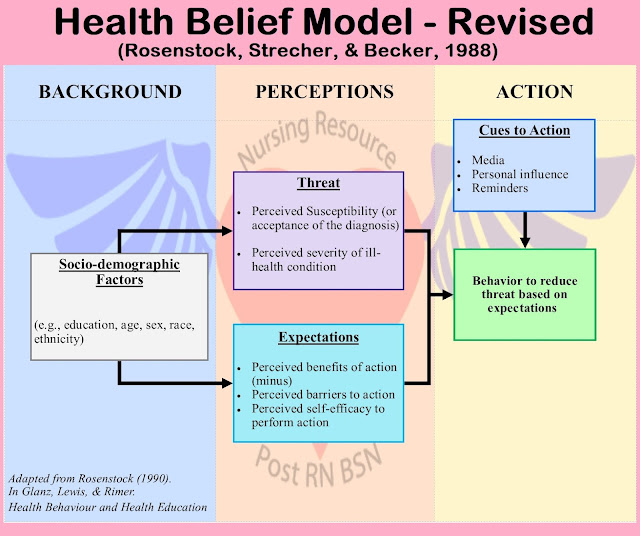
These concepts were proposed as accounting for people's "readiness to act." An added concept, cues to action, would activate that readiness and stimulate overt behavior. A current addition to the HBM is the concept of self-efficacy, or one's confidence in the ability to successfully perform an action. This concept was added by Rosenstock and others in 1988 to help the HBM better fit the challenges of changing habitual unhealthy behaviors, such as being sedentary, smoking, or overeating.
1 – Perceived Susceptibility
- Individuals who do not think they will get the flu are less likely to get a yearly flu vaccine.
- People who think they are unlikely to get skin cancer are less likely to apply sunscreen
- People who do not think that they are at risk of acquiring HIV from unprotected intercourse are less likely to use a condom.
- Young people who don't think they're at risk of lung cancer are less likely to stop smoking.
2 - Perceived Severity
- If a couple in love, are unlikely to avoid kissing on the mouth just because one have sniffles and other might get cold. On the contrary, one probably would stop kissing if it might give a more serious illness.
- Likewise, fewer people are likely to consider condoms when they think Sexually Transmitted Diseases are a minor problem. Therefore receptiveness to messages about safe sex increased during the AIDS epidemic. The perceived severity increased massively.
3 – Perceived Benefits
- A smoker probably won't give up, if don't think that doing so will improve their life in some way.
- A couple might not choose to exercise safe sex if they don't see how it could make their sex life healthier.
- People might not get vaccinated if they do not think there is a discrete benefit for them.
4 – Perceived Barriers
- Danger
- Expense
- Discomfort
- Inconvenience
- Social consequences
- Amount of effort required
- If everyone social group goes out drinking on Saturdays, it may be very difficult to cut down on one person’s alcohol intake.
- If a person think that condoms are a sign of mistrust in a relationship, he may be doubtful to bring them up.
















2 Comments
Hello, I have gone through your article and I found it really very informative. You know, you write the same thing which I was searching for. Thanks a lot for your efforts. Keep Posting dear. If anyone wants to enroll in an Nursing Definition, visit Virohan for that.
ReplyDeleteMy HSV2 Journey, A Natural Healing Success
DeleteI was diagnosed with HSV2 14 years ago, and honestly, it was pretty overwhelming at first. I got some info about tablets to help manage the outbreaks, but i was on a mission to find a natural remedy. As someone who loves hitting the gym and navigating the usual life stresses, I was facing outbreaks almost every month that could last for weeks.
I tried just about everything. Tea tree oil? Ouch, that stuff stung like crazy. Lysine? Sometimes it helped, but I had to take over 6000 mg daily, which just left me exhausted. Hot baths didn’t do anything for me either. I noticed that smoking and drinking seemed to trigger outbreaks, so I decided to cut those out since they weren’t doing my health any favors in my mid-30s.
Even regular exercise would lead to more outbreaks, and let’s not even talk about manscaping, definitely a no go. On top of all that, my mood was sinking, and I was feeling pretty down. My sex life was non existent, and I just wanted to feel like myself again. I wasn't a fan of prescription meds, and I was avoiding doctors because, you know, manly reasons. But I finally thought, why not?
After reading some great reviews online about Dr Utu Herbal Cure
, I decided to give it a shot. I reached out through his email at drutuherbalcure@gmail.com and ordered the Herpes Herbal Cleanser. I received the herbal cleanser through DHL and committed to a four week treatment plan.
Fast forward to when I got my blood tested, it came back negative for HSV2! I even went to another hospital for a second test, and once again, NEGATIVE! This was a total game changer for my health, and I can’t believe how quickly 13+ years of depression lifted.
Feeling like myself again has been truly incredible!